To join or leave the listserv visit https://scinfo.org/newsletter/
A Year In, 1st Patient To Get Gene Editing For Sickle Cell Disease Is Thriving
Since receiving a landmark treatment with the gene-editing tool CRISPR, a sickle cell patient has the strength to care for herself and her children — while navigating the pandemic.
Read in NPR: https://apple.news/A732Gi2ZuTiabNX7QKC22EA
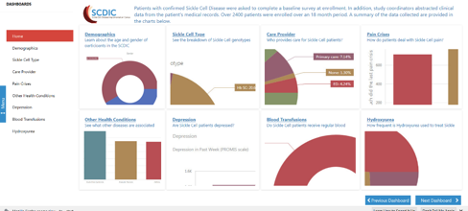
New Data Resource link for the Registry data collected by the Sickle Cell Disease Implementation Consortium https://scdicdashboard.azurewebsites.net/?mode=viewer&dashboardId=DashboardMenu
| World Sickle Cell Awareness Day on June 19, was first celebrated in 2009 and continues to be a great opportunity for organizations around the world and the sickle cell disease (SCD) global community to raise public awareness about the disease. Today, the American Society of Hematology (ASH) is proud to share significant progress in the Society’s transformative, multi-faceted, patient-centric initiative to improve outcomes for individuals with the disease, both in the United States and globally, by bringing together stakeholders in the public and private sectors committed to significantly improving the state of SCD worldwide. The following includes highlights of tools and programs ASH has created to help improve the lives of individuals living with SCD worldwide. We encourage you to learn, spread the word, and take action today Addressing Global Issues Learn more about the Consortium on Newborn Screening in Africa for SCD (CONSA), an ASH-supported collaboration to increase capacity for newborn screening, education, and clinical interventions for SCD in sub-Saharan Africa. Watch this video to learn more about ASH’s Global SCD Initiative. |
| Improving Patient Care Read about the ASH Clinical Practice Guidelines on Sickle Cell Disease – a series of guidelines with recommendations on the treatment of and complications stemming from SCD, including management of pain released today. View the new Resources for Sickle Cell Disease Pain Management web page, which will help you stay up to date on news, resources, and articles about SCD and acute and chronic pain. View the recently released SCD and COVID-19-Related Resources: Checklist for individuals living with SCD presenting to the emergency department (ED) during the pandemic. The downloadable checklist was developed by SCD and ED experts to assist in the evaluation of individuals with SCD in the ED who present symptoms concerning for COVID-19 and/or complications of SCD and provides SCD-specific considerations for evaluation and treatment. Frequently asked clinical questions on COVID-19 and SCD as we learn more about the virus and how it impacts SCD. Join the Society’s advocacy with the U.S. Congress to improve SCD care by participating in ASH’s online advocacy campaign. Contact your Senators and Representative today and urge them to support the creation of a Medicaid demonstration program focused on improving comprehensive outpatient preventive and primary care for individuals with SCD. Advancing Research Learn more about the ASH Research Collaborative (ASH RC), a non-profit organization established by ASH that fosters collaborative partnerships to accelerate progress in hematology, with the goal of improving the lives of people affected by blood diseases, particularly SCD. Read more about the ASH RC Sickle Cell Disease Clinical Trials Network, which optimizes the conduct of clinical trials research in SCD and leverages the ASH RC Data Hub to collect key information and identify gaps to advance SCD research and treatment. Subscribe to the ASH RC SCD Community Update Newsletter to stay connected with the community and learn about ASH’s research efforts. Donate to the ASH Foundation – Gifts to the ASH Foundation have a tremendous impact on hematology in terms of supporting basic and clinical research, clinical care, and fostering the development of the next generation of caregivers and researchers in hematology. ASH is pursuing major initiatives in sickle cell disease, patient registries, precision medicine, immunology, and hematology workforce recruitment and retention, complementing the Society’s ongoing core competencies, including the ASH Minority Recruitment Initiative, research awards, career development and training, and global programs. Continue the conversation online! In honor of World Sickle Cell Day, ASH and the Sickle Cell Disease Coalition (SCDC) will be sharing messages and resources on social media and we encourage your organizations to help promote it. Help spread awareness about the critical need for blood donations, especially from donors of African descent, to help patients living with SCD. |
| Questions? Contact ASH Customer Service at customerservice@hematology.org, 866-828-1321 (U.S. Only), or 202-776-0544. |
IASCNAPA Scholarship Applications Now Available
The International Association of Sickle Cell Nurses and Professional Associates’ (IASCNAPA) Steven Christy and Christine H. Johnson Scholarship funds were established to provide stipends to people with sickle cell disease (SCD) attending post-secondary education. Steven Christy battled SCD and was a staunch SCD advocate during his life, and Dr. Christine H. Johnson was an SCD provider and advocate her entire medical career. Scholarships were established in their honor by family and friends. To apply for an IASCNAPA scholarship, go to www.iascnapa.org
Terumo BCT Releases “Smart Blood Toolkit”
Terumo BCT released a “Smart Blood Toolkit” to assist sickle cell disease (SCD) providers in the best practices for blood management and achieving desired HbS targets during automated red blood cell exchanges. This timely information was released to address the ongoing concerns regarding the national blood supply and potential risk for individuals with SCD who receive chronic transfusions.
CDC’s Sickle Cell Data Collection Program Announcements
The Centers for Disease Control and Prevention’s (CDC’s) Sickle Cell Data Collection (SCDC) program determines the number of people living with sickle cell disease (SCD) and monitors changes related to their health over time.
- Website Update: CDC redesigned its SCDC program website with a cleaner, more streamlined layout and improved navigation.
- Webinar: Stay tuned for a webinar about the importance of incorporating a palliative approach to SCD care on Wednesday, July 1, 2020. Join the email list to receive announcements about upcoming webinars.
- World Sickle Cell Day: CDC is sharing personal stories about SCD, blood donation resources, and videos about the many faces of SCD on June 19. Stay updated by following us on Twitter at @CDC_NCBDDD.
- Newsletter: Subscribe to The Bloodline to stay in the know about SCDC activities, data, presentations, and more. Past issues are available here.
Nigerian Sickle Cell Patients Thriving During the Pandemic
By Katie Odey and Chika Obasi

Oyiji Odey Sickle Cell Program, Nigeria
We have had the Covid-19 Pandemic for a little over 5 months. Although it affects everybody, the main focus has been taking better care of the most vulnerable among us. Sickle Cell sufferers would probably be on the top of the list. According to the Center for Disease Control, (CDC), “People who are immunocompromised” are susceptible to the disease and need to be closely monitored. Coronavirus disease 2019 (COVID-19) is a highly infectious disease that affects your respiratory system. It was first discovered in December 2019 in Wuhan, China, but has since spread across the world resulting in a global pandemic. As of May 2020, there have been over 4 million cases and over 3 million deaths.
In Nigeria, the incidence of COVID-19 is increasing on a daily basis due to the increasing availability of test kits across the country. With the total number of confirmed cases put at 5,621, 176 deaths, and 1,472 recoveries, we are taking extra precautions to keep our patients safe and healthy. Every sphere, including the economic and educational sector in Nigeria, have been adversely and negatively affected due to poor its lack of preparedness and poor disaster management. The presence of coronavirus has worsened the condition of things and further impoverished the citizens leading to increased susceptibility to the disease as a result of scarcity of adequate nutrition owing to the lockdown.
Caring for patients with sickle cell pose a different challenge considering the increased cases of the coronavirus in African. In his article, on mitigating the effects of the COVID 19 on Sickle Cell Disease in Africa, Dexter writes: “The current focus on the COVID-19 pandemic in Africa and resource mobilization provides unique opportunities for optimizing health services for people with sickle cell disease in Africa and improving surveillance.” (Dexter, 2020) For patients like ours, it is imperative to take proper steps to ensure their overall well-being. For the past twenty years, we have focused largely on preventative care and education. Patients get a monthly supply of multivitamins, folic acid, and over-the-counter pain medicines. Many have thrived.
It is no doubt that Nigeria is a “resource-poor“ nation owing to poor governance. At our center, however, we have been able to adopt the use of face mask by both clients and health care provider, handwashing with soap before entering the clinic, use of hand gloves, division of clients into groups so as to minimize unnecessary contact and maintain social distance (152 clients were seen over a period of 4 days). So far so good our clients are doing very well with none presenting with complaints suggestive of COVID -19.
In the coming months, Dr. Obasi will begin to provide acute care for some of our patients. We will be introducing the use of Hydroxyurea for ten of our patients and collecting data to see how well they do. That data will be shared among some researchers to help in guiding our transition to acute care. Our immediate need is to start work on our clinic and research center, and the goal is to provide more qualitative to properly manage the disease.
Hydroxyurea is a game-changer in the management of sickle cell disease because of its curative properties and at our center, we intend to adopt it as a part of the standard care of our clients. In Nigeria however, the use of hydroxyurea is not common so we intend to carry a clinical trial on 10 of our clients to ensure that it is safe and effective before making it an integral component of our treatment protocol. Clearly, the use of hydroxyurea has been associated with a decreased rate of hospitalization due to both acute and chronic sickle cell disease. and an overall improvement of the quality of life of our clients with SCD during and after the pandemic. No doubt our routine medications have been helpful, they are not curative. Our center hopes to be among the first few centers in Nigeria to successfully provide the relief that our patients need through the use of hydroxyurea. This will bring hope and smiles to the faces of our clients.
Mitigating the effect of the COVID-19 pandemic on sickle cell disease services in African countries. Daniel Dexter, David Simons, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7180020/
Help ASH American Society of Hematology fight sickle cell disease
As a way to assess the state of SCD since the 2016 report card was released, identify the greatest opportunities for improvement, and highlight actions needed to make a significant difference in SCD access to care, education, research, and global issues. This year, during Sickle Cell Awareness Month in September, we plan on releasing an updated report card, which will showcase how much progress has been made over the past two years, as well as how much work still needs to be done.
We have developed a survey that will help us determine where SCD currently stands. As an individual living with SCD or individual working in an area related to the disease, we ask that youtake this survey so that we can determine how well we are doing in four main areas: access to care, training and professional education, research and clinical trials, and global issues. Detailed instructions are included in the survey portal. You are asked to respond anonymously as individuals, not as representatives of your institution or organization.
We kindly request that you complete this survey by Monday, July 6. Please feel free to share the survey with others in the SCD community.
Many thanks,
Stephanie
Stephanie Kaplan
Deputy Director, Government Relations and Public Health
American Society of Hematology
2021 L Street, NW, Suite 900
Washington, DC 20036
(202) 776-0544, x5263
Articles in the medical literature
| Sickle Cell Trait and The Potential Risk of Severe Coronavirus Disease 2019- A Mini-Review Eur J Haematol. 2020 Jun 26. doi: 10.1111/ejh.13478. Online ahead of print. Authors Tawakalitu Abosede Kehinde 1 , Mayowa Azeez Osundiji 2 Affiliations 1 Central and Northwest London NHS Foundation Trust, The Kingswood Centre, 134 Honeypot Lane, Kingsbury, London, NW9 0QY, United Kingdom. 2 Division of Clinical and Metabolic Genetics, The Hospital for Sick Children, University of Toronto, 555 University Avenue, Toronto, ON, M5G1X8, Canada. PMID: 32589774 DOI: 10.1111/ejh.13478 Abstract Coronavirus Disease 2019 (COVID-19) pandemic is a rapidly evolving public health problem. The severity of COVID-19 cases reported hitherto has varied greatly from asymptomatic to severe pneumonia and thromboembolism with subsequent mortality. An improved understanding of risk factors for adverse clinical outcomes may shed some light on novel personalized approaches to optimize clinical care in vulnerable populations. Emerging trends in the United States suggest possibly higher mortality rates of COVID-19 amongst African Americans, although detailed epidemiological study data is pending. Sickle Cell Disease (SCD) disproportionately affect Black/African Americans in the United States as well as forebearers from sub-Saharan Africa, the Western Hemisphere (South America, the Caribbean, and Central America) and some Mediterranean countries. The carrier frequency for SCD is high amongst African Americans. This article underscores the putative risks that may be associated with COVID-19 pneumonia in sickle cell trait as well as potential opportunities for individualized medical care in the burgeoning era of personalized medicine. Keywords: Acute Chest Syndrome (ACS); Coronavirus Disease 2019 (COVID-19); Sickle Cell Disease (SCD); Sickle Cell Trait; Thromboembolism; Vaso-Occlusive Crisis (VOC). | ||
| Emotional Distress Among Parent Caregivers of Adolescents With Sickle Cell Disease: Association With Patients and Caregivers Variables J Health Psychol. 2020 Jun 26;1359105320935986. doi: 10.1177/1359105320935986. Online ahead of print. Authors Ayodeji A Bioku 1 , Jude U Ohaeri 2 , Stephen O Oluwaniyi 3 , Tinuke O Olagunju 4 , Gary A Chaimowitz 4 , Andrew T Olagunju 4 5 6 Abstract Evidence suggests that impairment in caregiver wellbeing can alter the quality of care in children with sickle cell disease. We examined 121 parent caregivers of adolescents with sickle cell disease for emotional distress and disruptions to caregiver lifestyle and interests. Participants were predominantly mothers 92(76%) with mean age, 43.59 (SD = 6.39) years. Four in every ten caregivers had emotional distress, and this was predicted by frequent hospital attendance and disruptions in caregiver lifestyle, relationships, and interests. Psychosocial support to promote resilience and adaptive coping-styles to deal with the stress from unforeseen crises, frequent hospital visits, and lifestyle disruptions are indicated to improve caregiver wellbeing. Keywords: adolescents; illness intrusiveness; parent caregivers; psychological distress; psychosocial burden; sickle cell disease. | ||
| Parents of Children With Sickle Cell Disease Are Interested in Preimplantation Genetic Testing J Pediatr. 2020 Jun 22;S0022-3476(20)30471-6. doi: 10.1016/j.jpeds.2020.04.027. Authors Monica Attia 1 , Shawn Kripalani 1 , Isha Darbari 2 , Robert Sheppard Nickel 3 Abstract Objective: To evaluate awareness of and attitudes toward preimplantation genetic testing (PGT) for sickle cell disease (SCD) among parents of children with SCD. Study design: Parents of children with SCD were given an educational handbook on PGT before a routine SCD clinic visit. After their clinic visit, parents were asked to complete an anonymous survey. Results: Of 83 patents approached, 67 (81%) completed the survey. Only 16 of the 67 parents (24%) were previously aware of PGT for SCD. After our clinic-based education, 65 of the 67 parents (97%) indicated that it was important or very important for parents of children with SCD to know about PGT. Among parents interested in having more children, 29 of 32 (91%) would personally consider using PGT if covered by insurance. Conclusions: Parents of children with SCD are generally not aware of PGT. When educated in clinic, parents viewed information on PGT as valuable. Pediatricians and other health care professionals should inform parents of children with SCD about this reproductive option. Keywords: assisted reproductive technology; genetic counseling; preimplantation genetic diagnosis; reproductive choices; sickle cell anemia. | ||
| Red Cell Exchange for Patients With Sickle Cell Disease: An International Survey of Current Practices Transfusion. 2020 Jun 24. doi: 10.1111/trf.15863. Online ahead of print. Authors Matthew S Karafin 1 , Jeanne E Hendrickson 2 , Haewon C Kim 3 , Aisha Kuliya-Gwarzo 4 , Monica B Pagano 5 , Ajay Perumbeti 6 , Patricia A Shi 7 , Yvette C Tanhehco 8 , Jennifer Webb 9 , Edward Wong 9 , Quentin Eichbaum 10 Abstract Introduction: Red cell exchange (RCE) therapy is increasingly used to treat patients with acute or chronic manifestations of sickle cell disease (SCD). However, little is known regarding the most safe and effective practice parameters associated with this particular therapy. Methods: A SCD subcommittee of members of the American Society for Apheresis (ASFA) developed a 122-question survey and administered it via email to other ASFA members. The survey inquired about clinical indications for treatment, practice patterns, and transfusion policies for RCE when used for patients with SCD. Results: Ninety-nine distinct institutions completed the survey. Twenty-one (21%) were from outside of the US. Twenty-two (22%) provided chronic transfusion therapy to >10 patients, and both adult (25%) and pediatric-focused services (20%) were represented. Common acute indications for RCE included acute chest syndrome, acute ischemic stroke, and pre-surgical prophylaxis. Common chronic indications included primary stroke prophylaxis, secondary stroke prophylaxis, and recurrent acute chest syndrome. Respondents most commonly set a post-RCE treatment target of 30% for the hematocrit and hemoglobin S levels, regardless of the therapeutic indication. Units for RCE were phenotypically matched in 95% of cases. About 40% of respondents reported using isovolemic hemodilution. Conclusions: This survey solicited the current practice variations in RCE from a diverse range of practice sites. Many sites reported similar practice patterns and challenges but some variations emerged. To our knowledge, this survey represents the largest and most in-depth investigation of the use of RCE for patients with SCD, and could inform future studies in the field. © 2020 AABB. 44 references Full-text links Wiley | ||
| Management of Hemoglobin Disorders During the COVID-19 Pandemic Front Med (Lausanne). 2020 Jun 9;7:306. doi: 10.3389/fmed.2020.00306. eCollection 2020. Authors Sanjana Fatema Chowdhury 1 , Saeed Anwar 2 Free PMC article Abstract The coronavirus disease 2019 (COVID-19) is an emerging infectious disease that has become a global public health concern after being first reported in China and has subsequently spread worldwide. It causes mild to severe respiratory illness with some flu-like symptoms. The causal virus behind this disease, SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2), conceivably attacks the receptors of the respiratory system of the human body but has no strict evidence of attacking the blood cells yet. However, patients with hemoglobin disorders (e.g., sickle cell anemia, thalassemia) are vulnerable to this global health situation due to their clinical complications. Such patients are generally more prone to viral and bacterial infections, which can worsen their physical condition. Some of these patients present immunocompromised conditions, e.g., splenectomized or post-transplant patients. Therefore, they should follow some preventive steps such as shielding as well as the general guidelines for the COVID-19 pandemic. Transfusion dependent patients require regular monitoring for iron overload, and iron chelation therapy may be stopped by the physician depending on the situation. This article reviews the management strategies and provides some crucial recommendations for people in the corner with hemoglobin disorders. Keywords: COVID-19; SARS-CoV-2; clinical management; hemoglobin; hemoglobinopathies; iron chelation therapy; sickle cell diseases; thalassemia. Copyright © 2020 Chowdhury and Anwar. 40 references Publication types Review Full-text links Frontiers Media SA Free PMC article | ||
| Hydroxyurea Dose Escalation for Sickle Cell Anemia in Sub-Saharan Africa N Engl J Med. 2020 Jun 25;382(26):2524-2533. doi: 10.1056/NEJMoa2000146. Authors Chandy C John 1 , Robert O Opoka 1 , Teresa S Latham 1 , Heather A Hume 1 , Catherine Nabaggala 1 , Phillip Kasirye 1 , Christopher M Ndugwa 1 , Adam Lane 1 , Russell E Ware 1 Affiliation Abstract Background: Hydroxyurea has proven safety, feasibility, and efficacy in children with sickle cell anemia in sub-Saharan Africa, with studies showing a reduced incidence of vaso-occlusive events and reduced mortality. Dosing standards remain undetermined, however, and whether escalation to the maximum tolerated dose confers clinical benefits that outweigh treatment-related toxic effects is unknown. Methods: In a randomized, double-blind trial, we compared hydroxyurea at a fixed dose (approximately 20 mg per kilogram of body weight per day) with dose escalation (approximately 30 mg per kilogram per day). The primary outcome was a hemoglobin level of 9.0 g or more per deciliter or a fetal hemoglobin level of 20% or more after 24 months. Secondary outcomes included the incidences of malaria, vaso-occlusive crises, and serious adverse events. Results: Children received hydroxyurea at a fixed dose (94 children; mean [±SD] age, 4.6±1.0 years) or with dose escalation (93 children; mean age, 4.8±0.9 years); the mean doses were 19.2±1.8 mg per kilogram per day and 29.5±3.6 mg per kilogram per day, respectively. The data and safety monitoring board halted the trial when the numbers of clinical events were significantly lower among children receiving escalated dosing than among those receiving a fixed dose. At trial closure, 86% of the children in the dose-escalation group had reached the primary-outcome thresholds, as compared with 37% of the children in the fixed-dose group (P<0.001). Children in the dose-escalation group had fewer sickle cell-related adverse events (incidence rate ratio, 0.43; 95% confidence interval [CI], 0.34 to 0.54), vaso-occlusive pain crises (incidence rate ratio, 0.43; 95% CI, 0.34 to 0.56), cases of acute chest syndrome or pneumonia (incidence rate ratio, 0.27; 95% CI, 0.11 to 0.56), transfusions (incidence rate ratio, 0.30; 95% CI, 0.20 to 0.43), and hospitalizations (incidence rate ratio, 0.21; 95% CI, 0.13 to 0.34). Laboratory-confirmed dose-limiting toxic effects were similar in the two groups, and there were no cases of severe neutropenia or thrombocytopenia. Conclusions: Among children with sickle cell anemia in sub-Saharan Africa, hydroxyurea with dose escalation had superior clinical efficacy to that of fixed-dose hydroxyurea, with equivalent safety. (Funded by the Doris Duke Charitable Foundation and the Cincinnati Children’s Research Foundation; NOHARM MTD ClinicalTrials.gov number, NCT03128515.). Copyright © 2020 Massachusetts Medical Society. Publication types Research Support, Non-U.S. Gov’t Associated data ClinicalTrials.gov/NCT03128515 Grant support ICRA 2016156/DDCF/Doris Duke Charitable Foundation/United States None/Cincinnati Children’s Research Foundation/International Full-text links Atypon | ||
| Thrombin Generation in Children With Sickle Cell Anemia Is Higher in the Presence of Platelets ⋆ and ⋆ Transfus Apher Sci. 2020 Jun 16;102852. doi: 10.1016/j.transci.2020.102852. Online ahead of print. Authors Neethu Menon 1 , Janna Journeycake 2 , Rong Huang 3 , Paul Riley 4 , Ayesha Zia 5 Abstract Cellular and plasma interactions underlie hypercoagulability in sickle cell anemia (SCA). In healthy adults, thrombin generation (TG), a biomarker of hypercoagulability, is similar in plasma with and without platelets. Studies investigating TG in SCA using platelet-poor plasma (PPP) show conflicting results. There are no studies in SCA simultaneously comparing TG using platelet rich plasma (PRP) and PPP. This prospective study compares TG in children with SCA, at steady state, in PPP versus PRP and investigates the association of predefined clinical variables with the difference between PRP and PPP. Our secondary aim was to investigate derangements in the protein C and S pathway measuring TG with and without thrombomodulin (TM). In forty-three paired samples from SCA patients, aged 2-15 years, TG in the presence of platelets was 5.9 % higher [1239 nmol/(min*L) (SD: 224.1) vs. 1151 nmol/(min*L) (SD 223.3); p = 0.026]. The difference was highest in the 6-10 year age group (9.5 %; SD 14.1) followed by the 2-5 year age group (5.4 %; SD 21.4). In a multiple linear regression model, age, gender, current use of hydroxyurea, degree of hemolysis and severity of pain crises were not predictive of the difference between PRP and PPP. In PPP, TG reduction after TM addition was 7.4 % (SD 16.8), signifying activated protein C resistance. In conclusion, TG in children with SCA aged 2-10 years is higher in the presence of platelets. TG using PRP along with TM addition may be a useful biomarker of hypercoagulability in this population. Keywords: Hypercoagulability; Platelets; Sickle cell; Thrombin generation. Copyright © 2020 Elsevier Ltd. All rights reserved. Conflict of interest statement Declaration of Competing Interest None. Full-text links Elsevier Science | ||
| Impact of Neuropathic Pain on Quality of Life in Adults With Sickle Cell Disease: Observational Study Hematol Transfus Cell Ther. 2020 Jun 16;S2531-1379(20)30067-5. doi: 10.1016/j.htct.2020.03.010. Online ahead of print. Authors Lismar Fernando Oliveira Dos Santos 1 , Milenna Wild Guimarães 1 , Abrahão Fontes Baptista 2 , Katia Nunes Sá 3 Free article Abstract Introduction: Knowledge on the characteristics of neuropathic pain in people with sickle cell disease (SCD) may help to provide more effective treatment procedures. Objective: To describe the characteristics of neuropathic pain in patients with sickle cell disease and identify the impact on their quality of life. Method: A cross-sectional study (CAAE 57274516.8.0000.5544) was conducted at a reference center in Salvador, Bahia, Brazil. The instruments used were the Brief Pain Inventory (BPI), the Douleur Neuropatique Questionnaire (DN-4), the Anxiety and Depression Hospital scale (ADH) and the abbreviated version of the World Health Organization of Quality of Life questionnaire (WHOQOL-brief). The Mann-Whitney test was used to evaluate the association between the scores (5% alpha). Results: A total of 100 adults with SCD participated in the study, 69.7% of whom had neuropathic pain. Anxiety was present in 99% of the sample and depression, in 100%. Patients with neuropathic pain had worse scores in all domains of quality of life (p < 0.05), but no association was found with pain intensity. Conclusion: Neuropathic pain was more frequent than nociceptive pain in adults with SCD and generated worse scores in all domains of quality of life. Anxiety and depression were present in patients with both types of pain. Keywords: Anxiety; Depression; Neuropathic pain; Quality of life; Sickle cell disease. Copyright © 2020 Associação Brasileira de Hematologia, Hemoterapia e Terapia Celular. Published by Elsevier Editora Ltda. All rights reserved. Full-text links Elsevier Science | ||
| Preliminary Evaluation of a mHealth Coaching Conversational Artificial Intelligence for the Self-Care Management of People With Sickle-Cell Disease Stud Health Technol Inform. 2020 Jun 16;270:1361-1362. doi: 10.3233/SHTI200442. Authors David-Z Issom 1 , Jessica Rochat 1 , Gunnar Hartvigsen 2 , Christian Lovis 1 Abstract Adherence to the complex set of recommended self-care practices among people with Sickle-Cell Disease (SCD) positively impacts health outcomes. However, few patients possess the required skills (i.e. disease-specific knowledge, adequate levels of self-efficacy). Consequently, adherence rates remain low and only 1% of patients are empowered enough to master the self-care practices. Health coaching and therapeutic patient education have emerged as new approaches to enhance patients’ self-management and support health behavior changes. This preliminary feasibility study examined patients’ perceived usefulness of the information provided by a chatbot we developed following patient-important requirements collected during our preliminary studies. Participants tested the chatbot and completed a post-test survey. A total of 19 patients were enrolled and 2 withdrew. 15 respondents (15/17, 88%) gave a score of at least 3/4 to the question “The chatbot contains all the information I need”. Results suggest that mHealth coaching apps could be used to promote the knowledge acquisition of recommended health behaviors related to the prevention of SCD main symptoms. Keywords: Chatbots; Patient Empowerment; Sickle-Cell Disease; mHealth. Full-text links IOS Press | ||
| Emergency Department Provider Survey Regarding Acute Sickle Cell Pain Management J Pediatr Hematol Oncol. 2020 Jun 19. doi: 10.1097/MPH.0000000000001843. Online ahead of print. Authors Olufunke Y Martin 1 2 , Sean M Thompson 1 2 3 , Aaron E Carroll 1 2 4 5 , Seethal A Jacob 1 2 4 6 Abstract Sickle cell disease (SCD) can lead to potentially devastating complications that occur secondary to vaso-occlusion. Current national clinical guidelines are largely based on expert opinion, resulting in significant variation of management. Provider awareness regarding emergency department (ED) management of vaso-occlusive crises (VOC) remains unknown. A 23-question assessment of VOC management was administered to all eligible ED providers at Riley Hospital for Children between September and November 2018. Univariate analyses were performed to evaluate responses between groups. Of 52 respondents comprised of ED staff attendings (27%), resident trainees (58%), and ED nurses (15%), the majority were not aware of SCD management guidelines being available. Approximately 54% of providers endorsed a high comfort level in managing VOC, with staff and nurses more likely to report this than trainees (P=0.02). Less than 10% of all providers knew the recommended timeframe from triage to initial medication administration. Prolonged time between pain assessments was reported by 25% of providers with a high comfort level in managing VOC, which was similar to providers with a lower comfort level (13%, P=0.217). Only one fourth of all respondents appropriately did not use vital signs as an indication of a patient’s pain level, and >10% reported not utilizing patient-reported pain scores. This was not significantly different between provider comfort levels (P=0.285 and 0.412, relatively). Our results suggest education regarding recommended practices was inadequate regardless of reported provider comfort. Further provider education and/or standardized ED VOC management guidelines may serve as areas for improvement in SCD care. Full-text links Wolters Kluwer | ||
| Abdominal Manifestations of Sickle Cell Disease Curr Probl Diagn Radiol. 2020 Jun 1;S0363-0188(20)30113-4. doi: 10.1067/j.cpradiol.2020.05.012. Online ahead of print. Authors Nikhar P Kinger 1 , Courtney C Moreno 2 , Frank H Miller 3 , Pardeep K Mittal 4 Abstract Sickle cell disease is a debilitating hematologic process that affects the entire body. Disease manifestations in the abdomen most commonly result from vaso-occlusion, hemolysis, or infection due to functional asplenia. Organ specific manifestations include those involving the liver (eg, hepatopathy, iron deposition), gallbladder (eg, stone formation), spleen (eg, infarction, abscess formation, sequestration), kidneys (eg, papillary necrosis, infarction), pancreas (eg, pancreatitis), gastrointestinal tract (eg, infarction), reproductive organs (eg, priapism, testicular atrophy), bone (eg, marrow changes, avascular necrosis), vasculature (eg, vasculopathy), and lung bases (eg, acute chest syndrome, infarction). Imaging provides an important clinical tool for evaluation of acute and chronic disease manifestations and complications. In summary, there are multifold abdominal manifestations of sickle cell disease. Recognition of these sequela helps guide management and improves outcomes. The purpose of this article is to review abdominal manifestations of sickle cell disease and discuss common and rare complications of the disease within the abdomen. Copyright © 2020 Elsevier Inc. All rights reserved. Publication types Review Full-text links Elsevier Science | ||
| Voxelotor Treatment Interferes With Quantitative and Qualitative Hemoglobin Variant Analysis in Multiple Sickle Cell Disease Genotypes Am J Clin Pathol. 2020 Jun 20;aqaa067. doi: 10.1093/ajcp/aqaa067. Online ahead of print. Authors Nicola J Rutherford-Parker 1 , Sean T Campbell 2 , Jennifer M Colby 1 3 , Zahra Shajani-Yi 1 3 Abstract Objectives: Voxelotor was recently approved for use in the United States as a treatment for sickle cell disease (SCD) and has been shown to interfere with the quantitation of hemoglobin (Hb) S percentage. This study aimed to determine the effect of voxelotor on the quantitation of hemoglobin variant levels in patients with multiple SCD genotypes. Methods: In vitro experiments were performed to assess the impact of voxelotor treatment on hemoglobin variant testing. Whole blood samples were incubated with voxelotor and then analyzed by routinely used quantitative and qualitative clinical laboratory methods (high-performance liquid chromatography [HPLC], capillary zone electrophoresis [CZE], and acid and alkaline electrophoresis). Results: Voxelotor modified the α-globin chain of multiple hemoglobins, including HbA, HbS, HbC, HbD-Punjab, HbE, HbA2, and HbF. These voxelotor-hemoglobin complexes prevented accurate quantitation of multiple hemoglobin species, including HbS, by HPLC and CZE. Conclusions: Technical limitations in quantifying HbS percentage may preclude the use of HPLC or CZE for monitoring patients treated with voxelotor. Furthermore, it is unclear whether HbS-voxelotor complexes are clinically equivalent to HbS. Consensus guidelines for reporting hemoglobin variant percentages for patients taking voxelotor are needed, as these values are necessary for determining the number of RBC units to exchange in acute situations. Keywords: GBT440; HbS percentage; Hemoglobin S; Interference; Oxbryta; Sickle cell disease; Voxelotor. © American Society for Clinical Pathology, 2020. All rights reserved. For permissions, please e-mail: journals.permissions@oup.com. Full-text links Silverchair Information Systems | ||
| American Society of Hematology 2020 Guidelines for Sickle Cell Disease: Management of Acute and Chronic Pain Blood Adv. 2020 Jun 23;4(12):2656-2701. doi: 10.1182/bloodadvances.2020001851. Authors Amanda M Brandow 1 , C Patrick Carroll 2 , Susan Creary 3 , Ronisha Edwards-Elliott 4 , Jeffrey Glassberg 5 , Robert W Hurley 6 7 , Abdullah Kutlar 8 , Mohamed Seisa 9 , Jennifer Stinson 10 , John J Strouse 11 12 , Fouza Yusuf 13 , William Zempsky 14 , Eddy Lang 15 Abstract Background: The management of acute and chronic pain for individuals living with sickle cell disease (SCD) is a clinical challenge. This reflects the paucity of clinical SCD pain research and limited understanding of the complex biological differences between acute and chronic pain. These issues collectively create barriers to effective, targeted interventions. Optimal pain management requires interdisciplinary care. Objective: These evidence-based guidelines developed by the American Society of Hematology (ASH) are intended to support patients, clinicians, and other health care professionals in pain management decisions for children and adults with SCD. Methods: ASH formed a multidisciplinary panel, including 2 patient representatives, that was thoroughly vetted to minimize bias from conflicts of interest. The Mayo Evidence-Based Practice Research Program supported the guideline development process, including updating or performing systematic reviews. Clinical questions and outcomes were prioritized according to importance for clinicians and patients. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used, including GRADE evidence-to-decision frameworks, to assess evidence and make recommendations, which were subject to public comment. Results: The panel reached consensus on 18 recommendations specific to acute and chronic pain. The recommendations reflect a broad pain management approach, encompassing pharmacological and nonpharmacological interventions and analgesic delivery. Conclusions: Because of low-certainty evidence and closely balanced benefits and harms, most recommendations are conditional. Patient preferences should drive clinical decisions. Policymaking, including that by payers, will require substantial debate and input from stakeholders. Randomized controlled trials and comparative-effectiveness studies are needed for chronic opioid therapy, nonopioid therapies, and nonpharmacological interventions. © 2020 by The American Society of Hematology. Full-text links Silverchair Information Systems | ||
| Association Between Hospital Admissions and Healthcare Provider Communication for Individuals With Sickle Cell Disease Hematology. 2020 Dec;25(1):229-240. doi: 10.1080/16078454.2020.1780737. Authors Robert M Cronin 1 2 3 , Manshu Yang 4 5 , Jane S Hankins 6 , Jeannie Byrd 7 , Brandi M Pernell 7 8 , Adetola Kassim 9 , Patricia Adams-Graves 10 , Alexis A Thompson 11 , Karen Kalinyak 12 , Michael DeBaun 7 , Marsha Treadwell 13 Abstract Objective: To test the hypothesis that caregivers’ or adult participants’ low ratings of provider communication are associated with more hospital admissions among adults and children with sickle cell disease (SCD), respectively. Secondarily, we determined whether there was an association between the caregivers’ or participants’ health literacy and rating of providers’ communication. Methods: Primary data were collected from participants through surveys between 2014 and 2016, across six sickle cell centers throughout the U.S. In this cross-sectional cohort study, 211 adults with SCD and 331 caregivers of children with SCD completed surveys evaluating provider communication using the Consumer Assessment of Healthcare Providers and Systems (CAHPS), healthcare utilization, health literacy, and other sociodemographic and behavioral variables. Analyses included descriptive statistics, bivariate analyses, and logistic regression. Results: Participants with better ratings of provider communication were less likely to be hospitalized (odds ratio (OR) = 0.54, 95% confidence interval (CI) = [0.35, 0.83]). Positive ratings of provider communication were associated with fewer readmissions for children (OR = 0.23, 95% CI = [0.09, 0.57]). Participants with better ratings of provider communication were less likely to rate their health literacy as lower (regression coefficient (B) = -0.28, 95% CI = [-0.46, -0.10]). Conclusions: Low ratings of provider communication were associated with more hospitalizations and readmissions in SCD, suggesting the need for interventions targeted at improving patient-provider communication which could decrease hospitalizations for this population. Keywords: Provider communication; consumer assessment of healthcare providers and systems; health care surveys; shared decision-making; sickle cell anemia; vulnerable populations. Full-text links Taylor & Francis | ||
| Risk Score to Predict Event-Free Survival After Hematopoietic Cell Transplant for Sickle Cell Disease Blood. 2020 Jun 9;blood.2020005687. doi: 10.1182/blood.2020005687. Online ahead of print. Authors Ruta Brazauskas 1 , Graziana M Scigliuolo 2 , Hai-Lin Wang 1 , Barbara Cappelli 3 , Anna Lisa Ruggeri 4 , Courtney D Fitzhugh 5 , Jane S Hankins 6 , Julie Kanter 7 , Joerg J Meerpohl 8 , Julie Ann Panepinto 1 , Damiano Rondelli 9 , Shalini Shenoy 10 , Mark C Walters 11 , John E Wagner 12 , John F Tisdale 13 , Eliane Gluckman 14 , Mary Eapen 1 Abstract We developed a risk score to predict event-free survival (EFS; the probability of being alive with donor engraftment) after allogeneic hematopoietic cell transplantation for sickle cell disease. The study population (n=1425) was randomly split into training (n=1070) and validation (n=355) cohorts. Cox regression models were built to identify and validate risk factors. Of 9 risk factors evaluated, 2 biologic risk factors were predictive for EFS: age at transplantation and donor type. Based on the training cohort, patients aged ≤12 years with an HLA-matched sibling donor were at lowest risk with 3-year EFS of 92% (95% CI 89-94), score=0. Patients aged ≥13 years with an HLA-matched sibling donor or ≤12 years with an HLA-matched unrelated donor were at intermediate risk (score=1; 3-year EFS 87%, 95% CI 82-91). All other groups, including patients of any age with a haploidentical relative or HLA-mismatched unrelated donor and patients aged ≥13 years with an HLA-matched unrelated donor were high risk (score=2 or 3; 3-year EFS 57%, 95% CI 50-64). These findings were confirmed in the validation cohort. This simple risk score may guide hematologists and patients with sickle cell disease who are considering allogeneic transplantation as a curative treatment relative to other available contemporary treatments. Copyright © 2020 American Society of Hematology. Full-text links Silverchair Information Systems | ||
| Vitamin D Supplementation Improves Health-Related Quality of Life and Physical Performance in Children With Sickle Cell Disease and in Healthy Children J Pediatr Health Care. 2020 Jun 5;S0891-5245(20)30120-6. doi: 10.1016/j.pedhc.2020.04.007. Online ahead of print. Authors Kelly A Dougherty, Joan I Schall, Chiara Bertolaso, Kim Smith-Whitley, Virginia A Stallings Abstract Introduction: No study determined if vitamin D supplementation improves health-related quality of life (HRQL) using pediatric Patient-Reported Outcomes Measurement Information System or physical functioning in type SS sickle cell disease (HbSS). Method: Subjects with HbSS (n = 21) and healthy subjects (n = 23) were randomized to daily oral doses (4,000 vs. 7,000 IU) of cholecalciferol (vitamin D3) and evaluated at 6 and 12 weeks for changes in serum 25 hydroxyvitamin D (25(OH)D), HRQL, and physical functioning. Results: In subjects with HbSS, significant reductions in pain, fatigue, and depressive symptoms and improved upper-extremity function were observed. In healthy subjects, significant reductions in fatigue and improved upper-extremity function were observed. Significant improvements in peak power and dorsiflexion isometric maximal voluntary contraction torques were observed in both groups. In subjects with HbSS, improved plantar flexion isometric maximal voluntary contraction torques were observed. Both groups saw significant improvement in their total Bruininks-Oseretsky Test of Motor Proficiency score. Discussion: Daily high-dose vitamin D supplementation for African American children with and without HbSS improved HRQL and physical performance. Keywords: Sickle cell disease; muscle strength; physical performance; quality of life; vitamin D supplementation. Copyright © 2020 National Association of Pediatric Nurse Practitioners. Published by Elsevier Inc. All rights reserved. Full-text links Elsevier Science | ||
| Integrative Approaches to Treating Pain in Sickle Cell Disease: Pre-clinical and Clinical Evidence Complement Ther Med. 2020 Jun;51:102394. doi: 10.1016/j.ctim.2020.102394. Epub 2020 May 11. Authors Varun Sagi 1 , Donovan A Argueta 2 , Stacy Kiven 2 , Kalpna Gupta 3 Free PMC article Abstract Sickle cell disease (SCD) is a genetic disorder characterized by hemolysis, end-organ damage, inflammation, and pain. Recurrent and unpredictable episodes of acute pain due to vaso-occlusive crises are a unique feature of SCD. Many patients also develop lifelong chronic pain. Opioids are the primary method of pain treatment in SCD; however, continued use is associated with several adverse effects. Integrative approaches to treating pain in SCD are increasingly being explored to prevent the side effects associated with opioids. In this review, we highlight the mechanisms of pain in SCD and describe mechanism-based integrative approaches for treating pain. Keywords: Pain; Sickle cell disease. Copyright © 2020 Elsevier Ltd. All rights reserved. Conflict of interest statement Declaration of Competing Interest Kalpna Gupta: Fera Pharmaceuticals LLC: Consultancy, Honoraria; Tautona Group: Consultancy, Honoraria; Novartis advisory group: Honoraria; CSL Behring, honoraria; Grifols, Research Grant; 1910 Genetics, Resaerch Grant. All other authors declare no conflict of interest. Publication types Review Grant support R01 HL147562/HL/NHLBI NIH HHS/United States U01 HL117664/HL/NHLBI NIH HHS/United States Full-text links Elsevier Science | ||
Meetings for the Sickle Cell Community
2020 Indiana Sickle Cell Conference “Sickle Cell Trait: Taking a Closer Look” The new date September 25th. This one-day Sickle Cell Disease conference will feature educational sessions for healthcare providers, patients/families, and social services providers. The morning sessions will be devoted to healthcare providers and the afternoon sessions will be tailored for patients, family members and social workers. Medically oriented topics will include improving awareness about Sickle Cell Trait and some of the health complications that research indicates can be associated with it. Health care providers and others will be presented with information that will broaden current thinking about the prevalence of trait and its impacts on the human body. Patient oriented topics will include sessions on trait education, including the variant Sickle Cell genotypes and inheritance patterns. Both sessions are open to the public. All attendees will be provided with information about available resources and current trends in the field.
registration link… https://www.eventbrite.com/e/2020-indiana-sickle-cell-conference-tickets-95286583737
First IASCNAPA Conference
The International Association of Sickle Cell Nurses and Professional Associates (IASCNAPA) Sickle Cell Conference: Treating the Whole Person scheduled for 4/17/2020 in Memphis is cancelled due to COVID-19 concerns. The decision to cancel the conference took into account many important factors, including the risk of unnecessary exposure to our patient population.
The event is rescheduled for April 9, 2021 at the Memphis Hilton.
Your understanding and support are greatly appreciated! For information go to www.iascnapa.org
Foundation for Sickle Cell Disease Research Symposium
Due to the unprecedented Novel Coronavirus COVID-19, our annual in-person Symposium is rescheduled to September 23 – 25, 2020.
The Foundation for Sickle Cell Disease Research (FSCDR) is committed to supporting innovative research in sickle cell disease (SCD) to help maximize quality of life and improve survival for the generations of people affected by SCD. The Symposium focuses on interactive education, sharing of best practices, and exploring novel Learn more and register today. https://fscdr.org/the-symposium/


