Sickle Cell News for September 2020– To join or leave the listserv visit https://scinfo.org/newsletter/
September is Sickle Cell Month
The Howard University’s1867 Health Innovations Project and Center for Sickle Cell Disease have entered into a new partnership with the U.S. Department of Health and Human Services (HHS) aimed at finding ways to use technology and data to improve the everyday lives of patients with sickle cell disease, or SCD. https://newsroom.howard.edu/newsroom/article/13031/howard-university-and-hhs-announce-sickle-cell-partnership-address-patient
“Sickle cell disease is the most common genetic disease in the United States and primarily affects African Americans and other people of African descent,” said James G. Taylor VI, M.D., director of the Howard University Center for Sickle Cell Disease. “It leads to anemia, pain crisis, strokes, and other problems. We are excited to partner with HHS to use technology and data to address the long-standing challenges that patients with sickle cell disease face.”
To kick off the three-year partnership, Howard University and Health and Human Services will hold a new sickle cell disease innovation contest, called the Health+ Sickle Cell Disease Healthathon. The virtual event will take place Sept. 7-25. Patients, advocates, clinicians, researchers, designers, technologists, government employees, payers, policymakers, and members of the public will be invited to participate.
“HHS is working with Howard University to bring data-driven insights to a disease that deserves attention, innovation, and tech solutions. For far too long, people have suffered stigmatization and daily pain from this disease. Together, we can modernize sickle cell treatment and help people live better lives with sickle cell disease,” said Admiral Brett P. Giroir, M.D., Assistant Secretary for Health at HHS.
Participants in the Health+ SCD Healthathon will be invited to develop and prototype solutions and ideas in response to specific challenges affecting patients with sickle cell disease, such as barriers in hospital emergency rooms and transition to adulthood. The prototype solutions and ideas will be reviewed by judges and contest winners will be awarded on Sept. 25 during a Healthathon Finale event. Learn more here
“The strategic partnership with HHS will identify and support opportunities for the government and private sector to accelerate meaningful innovation and technology solutions that address the challenges patients with SCD face on a daily basis,” said Michael Crawford, associate dean for strategy, outreach, and innovation at the Howard University College of Medicine.
The new sickle cell partnership will tackle long-standing challenges related to care for individuals and families affected by the disease: patient transition from pediatric to adult medicine, improving care during emergency department visits, enhancing patient and family engagement, and strengthening overall care coordination for sickle cell patients. About 100,000 Americans suffer from some form of the disease.
Under the partnership, the 1867 Health Innovations Project and the Center for Sickle Cell Disease will take the lead in gathering and collecting datasets related to or containing a subset of detail relevant to SCD, securing confirmation of data usage during the Healthathon event, and providing technology, innovation, and SCD expertise to promote the broad interest of the Healthathon.
The Center for Sickle Cell Disease, the Howard University College of Medicine, and Howard University Hospital have long served as a major international center for medical care, research, and other resources for people with sickle cell disease. Howard University’s Center for Sickle Cell Disease was founded in 1972 by the late Roland B. Scott, M.D., and has a distinguished history of leading clinical investigation in sickle cell disease.
Howard University launched the 1867 Health Innovations Project in April. Aptly named after the year the University was founded, 1867 aims to collaborate with innovators, entrepreneurs, researchers, and corporate partners to tackle complex health challenges confronting underserved populations in the Washington, D.C. region and beyond.
For more information about the 1867 Health Innovations Project, contact Michael Crawford, associate dean in the Howard University College of Medicine, michael.crawford@howard.edu
The Sickle Cell Foundation Of Tennessee Launches Sickle Cell Today Podcast On The KUDZUKIAN Network
On the heels of a series of successful virtual webinars, The Sickle Cell Foundation of Tennessee will launch the Sickle Cell Today podcast on the KUDZUKIAN Network. The first of the four episode series debuted on Monday, August 10th and will air once a week going forward. Episodes will focus on pain management, quality of life, treatments, and coping among other topical issues. Featured guests include Dr. Patricia Adams-Graves and Tabatha Marmon, a sickle cell disease patient advocate, among other industry experts and advocates.
Sickle Cell Disease is the most common inherited blood disorder affecting about 100,000 Americans, most often affecting people of African Americans/people of African descent followed closely by Hispanic-Americans from Central and South America and people of Mediterranean, Asian, Indian, or Middle Eastern descent. It can manifest in a myriad of ways, ranging from mild pain and discomfort to days and weeks of debilitating pain, stroke, or organ damage.
Reginald French, the president and CEO of The Sickle Cell Foundation of Tennessee, will serve as the host of the show. French says,
“We are excited about being able to extend our reach in this week. Great is the need in our community. We have some of the most highly regarded doctors within the specialty area serving as subject matter experts. They have a wealth of knowledge, recommendations and real-life solutions to share with listeners.”
Sickle Cell Today which can be accessed at https://sicklecelltoday.kudzukiannetwork.com. It also available on all streaming platforms – Spotify, Google Chrome, Apple, iHeart, Pandora.
Adding Sickle Cell Disease To FDA’s Priority Review Voucher List Of Neglected Tropical Diseases https://www.forbes.com/sites/joshuacohen/2020/08/18/adding-sickle-cell-disease-to-fdas-priority-review-voucher-list-of-neglected-tropical-diseases/#6241802ae6ee
On July 16th, Putting Rare Diseases Patients First!® filed a citizen’s petition to add sickle cell disease to the Food and Drug Administration’s priority review voucher list of neglected tropical diseases. Dr. Lorna Speid, founder and president of the non-profit that supports patients with rare and neglected diseases, says her organization took the action because sickle cell disease is the only tropical disease that afflicts a majority African American population in the U.S.
Priority review vouchers for neglected tropical diseases are aimed to incentivize pharmaceutical companies to develop drugs and vaccines for such diseases. Priority reviews of new drug applications take six months to complete, rather than the standard review period of 10 months. Typically, the priority review designation is given to drugs that treat serious diseases and provide a significant improvement compared to existing therapies.
To qualify for a priority review voucher, a sponsor’s application must be for a drug, biologic, or vaccine for the prevention or treatment of a neglected tropical disease. Sickle cell disease fits the bill of a neglected tropical disease.
Sickle cell disease constitutes a group of congenital red blood cell disorders, named sickle cell for the crescent shape of red blood cells. Sickle cell disease alters the structure of hemoglobin, the molecule in red blood cells that delivers oxygen to organs and tissue throughout the body. The most common disorder type is sickle cell anemia. Sickle cell disease causes significant morbidity, including severe pain, anemia, organ damage, and infections. The disease also leads to premature mortality.
In the U.S., approximately 100,000 patients are living with the congenital disease. The disease predominantly impacts people of sub-Saharan African descent.
Of the 20 million patients suffering from sickle cell disease worldwide, most reside in Africa. Many of these patients lack newborn screening for the disease, and access to even the most basic of treatments, such as hydroxyurea.
For a sponsor, a neglected tropical disease priority review voucher offers a six-month expedited review of another drug in the sponsor’s development pipeline if it gains approval for a drug with a neglected disease indication. Alternatively, the voucher can be sold to another company. Though critics have claimed that the program doesn’t require treatments to be novel or affordable, the program has been successful in ensuring development and launch of a number of important, new medications for neglected tropical diseases.
Be The Match Atlanta Encourages Donors to Join The Registry During African-American Bone Marrow Awareness Month
Black or African-American patients only have a 23% chance of finding a match compared to a 77% chance for White patients.
For too long, the Black/African-American community has sought a cure for sickle cell anemia, leukemia and other blood cancers. Well, there is a cure —a blood stem cell transplant from a genetically matched donor of a similar ethnic background. Yet of the 22 million potential donors on the Be The Match Registry, only 4% are Black or African-American.
One such patient that is in need is 10-year-old Ava of Snellville, Ga., who had her first pain crisis from sickle cell disease when she was just 5 months old. Over the past decade, she has been hospitalized over 70 times, and has had her spleen, adenoids, tonsils and gall bladder removed as a result of complications from sickle cell disease. A blood stem cell or bone marrow transplant from a perfectly matched donor is the only cure for sickle cell disease, but Ava does not have a compatible match in her family or on the Be The Match Registry.
Donors who have stepped up to the plate are encouraging others to do so. Tunisia Thorne, an Atlanta realtor, mom and wife who loves to volunteer, joined the registry in 1999 in San Diego by simply swabbing her cheek. Thorne got the call 18 years later, in 2017, that she was a perfect match. Thorne’s donation saved a 27-year old young man with leukemia.
“This is the epitome of Black lives matter,” said Thorne. “It is so very simple. It doesn’t take anything away from you, and it gives something so beautiful: life.”
Richard Stewart, an athletic trainer for Georgia Tech, swabbed at an athletic training convention in 2018. He didn’t think much about it, just heard there was a need and thought, “Why not?” Just four months later he got the call saying he was a potential match. He donated in January 2019.
“The whole process was phenomenal. The actual donation day was the same way, people treat you like a hero, even though I don’t consider myself a hero,” Stewart said. “I would do it again in a heartbeat, and would encourage others to do so.” Stewart’s donation saved a 63-year-old woman with acute myeloid leukemia (AML).
Like 80% of donors, Thorne and Stewart both donated through Peripheral Blood Stem Cell (PBSC) donation, a nonsurgical process similar to donating plasma.
“We are asking for Black Atlantans, particularly during African-American Bone Marrow Awareness Month, to help those in our community who are suffering from blood cancers and sickle cell,” said Xavier Brandon, Be The Match representative. “You will only be asked to donate if you are identified as a perfect match for a patient in need – some people receive the call in months, others after several years and many are never called to donate. But it only takes a simple cheek swab to increase the odds of a patient finding their perfect match. You can provide hope for people fighting for their lives.”
To find out more information about how to join the registry visit: https://www.bethematchatl.org.
Articles in the medical literature
| 1. An Interrupted Time Series Analysis of the Dissemination of a Sickle Cell Vaso-Occlusive Episode Treatment Algorithm and a Case Management Referral Form for Individuals With Sickle Cell Disease in the Emergency Department J Emerg Nurs. 2020 Aug 18;S0099-1767(20)30170-7. doi: 10.1016/j.jen.2020.06.001. Online ahead of print. Authors Dominique Bulgin, Emily Bonnabeau, Angie Alexander, Emilia Frederick, Gary Rains, Nirmish Shah, Matthew Young, Paula Tanabe Background: Sickle cell disease is associated with frequent vaso-occlusive episode and emergency department visits. Our group developed (1) a vaso-occlusive episode treatment algorithm based on the National Heart, Lung, and Blood Institute recommendations, and (2) a case management referral form to identify social behavioral health needs of patients with sickle cell disease in the emergency department. The aims of this project were to (1) disseminate the vaso-occlusive episode algorithm and case management referral form, and (2) to evaluate the individual provider-reported awareness, use, and preferred method of access to each tool among emergency department providers in North Carolina. Methods: An interrupted time series analysis was used to study the impact that an educational effort had on the awareness of a sickle cell vaso-occlusive episode treatment algorithm and a case management referral form. A targeted list was developed to identify the providers working in emergency departments with the largest number of sickle cell disease patient visits. In-service education was provided to targeted emergency departments in North Carolina over a period of 3 years. The vaso-occlusive episode algorithm and case management referral form were put up on the websites of professional organizations. Surveys were provided to emergency department providers at these targeted emergency departments with a baseline and post dissemination at 20 and 32 months for assessing the provider awareness, use, and preferred method of access of the tools. Additional feedback could be given by the participants through telephone interviews. Descriptive statistics were obtained, and content analysis was performed on interviews. Results: We received survey responses for the following periods: baseline (T1, n = 190), post dissemination at 20 (T2, n = 142), and 32 months (T3, n = 93). Awareness of the tools was between 42% (baseline) and 41% (post dissemination at T2, T3) for the vaso-occlusive episodes algorithm and 25% (baseline) and 29% (post dissemination at T2, T3) for the case management referral form. However, use of these tools was found to be low as only 19% of the emergency department providers used the vaso-occlusive episode algorithm at T1 and 13% T2, while 5% of emergency department providers used the case management referral form at T1 and 6% at T2. With further education about the tools, an increase in the usage of the tools was observed T3, which was 29% for the vaso-occlusive episodes algorithm and 9% for the case management referral form. Lack of incorporation of the decision support tools into emergency department processes was observed to be an overarching barrier to dissemination of the tools identified in interviews (n = 8). Conclusions: This study can be used to inform future strategies on dissemination of evidence-based tools to emergency department providers. Keywords: Case management; Decision support tools; Dissemination and implementation science; Emergency department; Sickle cell disease; Vaso-occlusive episode. Copyright © 2020 Emergency Nurses Association. Published by Elsevier Inc. All rights reserved. 2. Splenic Infarct Secondary to High Altitude Exposure in Sickle Cell Trait Patients: A Case Series Cureus. 2020 Aug 17;12(8):e9815. doi: 10.7759/cureus.9815. Authors Luis Gonzalez 1 , Andres F Shapiro 2 , Alfonso Tafur 3 , Carlos Plaza-Meneses 2 , Brenner Sabando 4 Abstract The sickle cell trait is considered a benign entity that generally does not show clinical manifestations. However, some complications have been described under certain conditions, such as a decrease in oxygen level, dehydration, and strenuous physical efforts. Among them, splenic infarct is a rare complication that presents as left upper abdominal pain in a situation of stress such as high altitude exposure. We present two cases of splenic infarcts in patients with undiagnosed sickle cell trait who showed to our institution with severe abdominal pain after coming from high altitude cities. Keywords: high altitude; sickle cell trait; splenic infarct. Copyright © 2020, Gonzalez et al. Conflict of interest statement The authors have declared that no competing interests exist. 20 references 2 figures 3. Primary prevention of sickle cell disease using preimplantation genetic testing and in vitro fertilization is cost-effective Am J Hematol. 2020 Aug 20. doi: 10.1002/ajh.25974. Online ahead of print. Authors Christina N Cordeiro Mitchell 1 2 3 , Apoorva Pradhan Bams 4 , Bhuchitra Singh 5 2 , Rakhi P Naik 6 , Valerie L Baker 1 2 , Sophie M Lanzkron 6 , Mindy S Christianson 1 2 , Lydia H Pecker 2 6 Abstract For couples with sickle cell trait (SCT) who are at risk for having a child with sickle cell disease (SCD), cost is a barrier to using in vitro fertilization (IVF) with preimplantation genetic testing for monogenic diseases (PGT-M) and insurance coverage is not universal. The objective of this study was to evaluate the cost-effectiveness of IVF+PGT-M for couples who both carry SCT and wish to avoid SCD in a child compared to natural conception with the possible birth of a child with SCD, and the associated lifetime medical costs and lost income. A cost-effectiveness analysis was performed with a decision analytic model. Sensitivity analyses, including Monte Carlo Simulations, assessed the impact of changes in input parameters on the incremental cost-effectiveness ratio (ICER). Probabilities and cost estimates were derived from the published literature. Effectiveness was measured in life years (LY) gained. The ICER was calculated to determine the cost-effectiveness of the IVF+PGT-M intervention. Compared to natural conception, IVF+PGT-M had an effectiveness gain of 30 LY, an additional cost of $572,392.68 per individual conceived, and an ICER of $19,319 per LY gained. The ICER is lower than a conservative, preset willingness to pay (WTP) threshold of $50,000 per LY gained. Monte Carlo Simulations demonstrated that, in 91% of iterations, IVF+PGT-M was cost-effective at the WTP of $50,000. IVF+PGT-M is a cost-effective strategy to avoid conceiving a child with SCD and broader insurance coverage is warranted. This article is protected by copyright. All rights reserved. 4. The molecular basis for the prothrombotic state in sickle cell disease Haematologica. 2020 Aug 13;haematol.2019.239350. doi: 10.3324/haematol.2019.239350. Online ahead of print. Authors Arun S Shet 1 , Maria A Lizarralde-Iragorri 2 , Rakhi P Naik 3 Abstract The genetic and molecular basis of sickle cell disease (SCD) has long since been characterized but the pathophysiological basis is not entirely defined. How a red cell hemolytic disorder initiates inflammation, endothelial dysfunction, coagulation activation and eventually leads to vascular thrombosis, is yet to be elucidated. Recent evidence has demonstrated a high frequency of unprovoked/recurrent venous thromboembolism (VTE) in SCD, with an increased risk of mortality among patients with a history of VTE. Here, we thoroughly review the molecular basis for the prothrombotic state in SCD, specifically highlighting emerging evidence for activation of overlapping inflammation and coagulation pathways, that predispose to venous thromboembolism. We share perspectives in managing venous thrombosis in SCD, highlighting innovative therapies with the potential to influence the clinical course of disease and reduce thrombotic risk, while maintaining an acceptable safety profile. 5. Management of chronic respiratory complications in children and adolescents with sickle cell disease Eur Respir Rev. 2020 Aug 18;29(157):200054. doi: 10.1183/16000617.0054-2020. Print 2020 Sep 30. Authors Michele Arigliani 1 2 , Atul Gupta 3 4 Abstract Sickle cell disease (SCD) is a life-threatening hereditary blood disorder that affects millions of people worldwide, especially in sub-Saharan Africa. This condition has a multi-organ involvement and highly vascularised organs, such as the lungs, are particularly affected. Chronic respiratory complications of SCD involve pulmonary vascular, parenchymal and airways alterations. A progressive decline of lung function often begins in childhood. Asthma, sleep-disordered breathing and chronic hypoxaemia are common and associated with increased morbidity. Pulmonary hypertension is a serious complication, more common in adults than in children. Although there is a growing attention towards respiratory care of patients with SCD, evidence regarding the prognostic meaning and optimal management of pulmonary issues in children with this condition is limited.This narrative review presents state-of-the-art evidence regarding the epidemiology, pathophysiology and therapeutic options for chronic respiratory complications commonly seen in paediatric patients with SCD. Furthermore, it highlights the gaps in the current knowledge and indicates future directions for studies that aim to improve our understanding of chronic respiratory complications in children with SCD. 6. Physical Therapy in Pediatric and Young Adult Patients With Sickle Cell Disease: Assessing Potential Benefits and Barriers J Pediatr Hematol Oncol. 2020 Aug 18. doi: 10.1097/MPH.0000000000001888. Online ahead of print. Authors Daniel Callaway 1 , Anjulika Chawla 2 , Philippa Sprinz 2 Abstract Background: Despite advances in the treatment of sickle cell disease (SCD) in pediatric and young adult patients, pain remains a significant cause of disease-related morbidity. Physical therapy has been shown to be useful for the treatment of pain in young patients with chronic illnesses, however, limited data exists regarding potential benefits of physical therapy in patients with SCD. Materials and methods: We conducted a web-based survey of health care providers and support staff in the New England area to identify potential benefits of and barriers to outpatient physical therapy in this patient population. Results: Nearly 92% of survey participants felt that physical therapy had the potential to be beneficial in pediatric and young adult patients with SCD. A majority of physicians reported having referred patients with SCD for physical therapy. Perceived potential benefits included improved functional mobility, improved chronic pain symptoms, decreased opiate use, improved mood symptoms, improved acute pain symptoms, and improved adherence with medications and clinic visits. Significant perceived barriers identified included lack of transportation, time constraints, patient lack of understanding, and difficulty with insurance coverage. Conclusions: Health care providers have a positive view of the use of physical therapy in the management of this patient population. Significant barriers exist which need to be addressed. 7. Vaso-occlusive crises and costs of sickle cell disease in patients with commercial, Medicaid and Medicare Insurance – The perspective of private and public payers J Med Econ. 2020 Aug 20;1. doi: 10.1080/13696998.2020.1813144. Online ahead of print. Authors Nirmish R Shah 1 , Menaka Bhor 2 , Dominick Latremouille-Viau 3 , Vikash Kumar Sharma 4 , Gary A Puckrein 5 , Patrick Gagnon-Sanschagrin 3 , Ankur Khare 4 , Mukesh Kumar Singh 4 , Elizabeth Serra 3 , Mikhaïl Davidson 3 , Liou Xu 5 , Annie Guerin 3 Abstract Aim: To characterize vaso-occlusive crises (VOCs) and describe healthcare costs among commercially-insured, Medicaid-insured, and Medicare-insured patients with sickle cell disease (SCD).Materials and Methods: The IBM Truven Health MarketScan Commercial (2000-2018), Medicaid Analytic eXtract (2008-2014), and Medicare Research Identifiable Files (2012-2016) databases were used to identify patients with ≥2 SCD diagnoses. Study measures were evaluated during a 12-month follow-up period, stratified by annual number of VOCs (i.e., 0, 1, and ≥2).Results: Among 16,092 commercially-insured patients (mean age =36.7 years), 35.3% had 1+ VOCs. Mean annual total all-cause healthcare costs were $15,747, $27,194, and $64,555 for patients with 0, 1, and 2+ VOCs, respectively. Total all-cause healthcare costs were mainly driven by inpatient (0 VOC =31.0%, 1 VOC =53.1%, 2+ VOCs =65.4%) and SCD-related costs (0 VOC =56.4%, 1 VOC =78.4%, 2+ VOCs =93.9%).Among 18,287 Medicaid-insured patients (mean age =28.5 years, fee-for-service =50.2%), 63.9% had 1+ VOCs. Mean annual total all-cause healthcare costs were $16,750, $29,880, and $64,566 for patients with 0, 1, and 2+ VOCs, respectively. Inpatient costs (0 VOC =37.2%, 1 VOC =64.3%, 2+ VOCs =72.9%) and SCD-related costs (0 VOC =60.9%, 1 VOC =73.8%, 2+ VOCs =92.2%) accounted for a significant proportion of total all-cause healthcare costs.Among 15,431 Medicare-insured patients (mean age =48.2 years), 55.1% had 1+ VOCs. Mean annual total all-cause healthcare costs were $21,877, $29,250, and $58,308 for patients with 0, 1, and ≥2 VOCs, respectively. Total all-cause healthcare costs were mainly driven by inpatient (0 VOC =47.9%, 1 VOC =54.9%, 2+ VOCs =67.5%) and SCD-related costs (0 VOC =74.9%, 1 VOC =84.4%, 2+ VOCs =95.3%).Limitations: VOCs managed at home were not captured. Analyses were descriptive in an observational setting; thus, no causal relationships can be inferred.Conclusions: A high proportion of patients experienced VOCs across payers. Furthermore, inpatient and SCD-related costs accounted for a significant proportion of total all-cause healthcare costs, which increased with VOC frequency. 8. Abatacept is effective as GVHD prophylaxis in unrelated donor stem cell transplantation for children with severe sickle cell disease Blood Adv. 2020 Aug 25;4(16):3894-3899. doi: 10.1182/bloodadvances.2020002236. Authors Alexander Ngwube 1 , Niketa Shah 2 , Kamar Godder 3 , David Jacobsohn 4 , Monica L Hulbert 5 , Shalini Shenoy 5 Abstract We report results of a phase 1 multicenter stem cell transplantation (SCT) trial from HLA-matched (n = 7) or one-antigen-mismatched (n = 7) unrelated donors (URD) using bone marrow or cord blood as stem cell source, following reduced-intensity conditioning (RIC) in severe sickle cell disease (SCD). Conditioning included distal alemtuzumab, fludarabine, and melphalan (matched donors), with thiotepa (mismatched donors). Abatacept, a selective inhibitor of T cell costimulation, was added to tacrolimus and methotrexate as graft-versus-host disease (GVHD) prophylaxis to offset GVHD risks, and was administered for longer duration in bone marrow recipients than in cord blood recipients because of increased incidence of chronic GVHD with bone marrow. Median age at transplant was 13 years (range, 7-21 years). The incidence of grades II to IV and grades III to IV acute GVHD at day +100 was 28.6% and 7%, respectively. One-year incidence of chronic GVHD was 57% and mild/limited in all but 1 patient who received abatacept for a longer duration. Only 1 patient developed reversible posterior encephalopathy syndrome and recovered. With a median follow-up of 1.6 years (range, 1-5.5 years), the 2-year overall and disease-free survival was 100% and 92.9%, respectively. The encouraging results from the phase 1 portion of this RIC SCT trial, despite risk factors such as older age, URD, and HLA-mismatch, support further evaluation of URD SCT in clinical trial settings. The phase 2 portion of the trial is in progress. This trial was registered at www.clinicaltrials.gov as NCT03128996. © 2020 by The American Society of Hematology. 9. Pica behaviors in pediatric patients with sickle cell disease: A scoping review protocol JBI Evid Synth. 2020 May 28. doi: 10.11124/JBISRIR-D-19-00241. Online ahead of print. Authors Olivia M Clark 1 , Renee Williams Abstract Objective: The objective of this review is to explore existing literature regarding pica in pediatric patients with sickle cell disease and to identify associated interventions and outcomes. Introduction: Pica is a psychological eating disorder that is characterized by the consumption of items that contain no nutritional value. The ingestion of non-food items causes complications that can be harmful or even fatal. Approximately one third of patients with sickle cell disease will also develop pica behaviors. Inclusion criteria: This review will consider studies that include pediatric patients from 18 months to 18 years of age who have been diagnosed with any type of sickle cell disease and have a history of pica. The study will examine interventions used in any setting to treat pediatric patients with sickle cell disease and pica and associated outcomes. Any study type will be considered for inclusion. Methods: An initial limited search of MEDLINE (PubMed) and CINAHL (EBSCO) will be performed to identify articles. Other databases to be searched will include CINAHL (EBSCO), Embase (Elsevier), Europe PubMed Central (PubMed), Psychology and Behavioral Sciences Collection (EBSCO), and Scopus (Elsevier). Data will be extracted from included papers by two independent reviewers. The data extracted will include details about the populations, concept, context, and study methods of significance to the review questions and objective. The extracted data will be presented in diagrammatic or tabular form in a manner that aligns to the objectives and scope of this review 10. Automated exchange compared to manual and simple blood transfusion attenuates rise in ferritin level after 1 year of regular blood transfusion therapy in chronically transfused children with sickle cell disease Transfusion. 2020 Aug 19. doi: 10.1111/trf.15982. Online ahead of print. Authors Shannon Kelly 1 2 , Mark Rodeghier 3 , Michael R DeBaun 4 Abstract Background: Optimal strategies for regular blood transfusion therapy are not well defined in sickle cell disease (SCD). This analysis tested the hypothesis that in the first of year of regular transfusions, when chelation therapy use is minimal, automated exchange transfusion would be the superior method for attenuating the rise in ferritin levels compared to simple and manual exchange transfusions. Study design and methods: The Silent Cerebral Infarct Multi-Center Clinical Trial randomly allocated children with SCD and silent cerebral infarcts to receive standard care or regular transfusions with a target pre-transfusion HbS concentration ≤ 30% and minimum hemoglobin level > 9.0 g/dL. Participants with at least nine transfusions and sufficient ferritin testing in the first year of the trial were included in a planned secondary analysis. Ferritin levels by the end of the first study year were compared between participants receiving automatic exchange transfusion, manual exchange transfusion, and simple transfusion. Results: A total of 83 participants were analyzed. During the first year of the study, 75.9% of the participants had >80% of transfusions via one transfusion method. At baseline no significant differences in ferritin levels were observed in the three transfusion groups (p = 0.1). After 1 year of transfusions the median (interquartile range) ferritin levels in the simple transfusion (n = 40), manual exchange transfusion (n = 34) and automatic exchange transfusion (n = 9) groups were 1800 ng/mL (1426-2204 ng/mL), 1530 ng/mL (1205-1805 ng/mL), and 355 ng/mL (179-579 ng/mL), respectively (p < 0.001). Conclusion: Automated exchange transfusion, when compared to other transfusion methods, is the optimal transfusion strategy for attenuating increase in ferritin levels in children with SCD. © 2020 AABB. 26 references 11. Fetal Hemoglobin in Sickle Cell Anemia Blood. 2020 Aug 17;blood.2020007645. doi: 10.1182/blood.2020007645. Online ahead of print. Author Martin H Steinberg 1 Abstract Fetal hemoglobin (HbF) can blunt the pathophysiology, temper the clinical course and offer prospects for curative therapy of sickle cell disease. This review focuses on: 1. HbF quantitative trait loci and the geography of β-globin gene haplotypes, especially those found in the Middle East; 2. how HbF might differentially impact the pathophysiology and many subphenotypes of sickle cell disease; 3. clinical implications of person-to-person variation in the distribution of HbF among HbF-containing erythrocytes; 4. reactivation of HbF gene expression using both pharmacologic and cell-based therapeutic approaches. A confluence of detailed understanding of the molecular basis of HbF gene expression, coupled with the ability to precisely target by genomic editing most areas of the genome, are producing important preliminary therapeutic results that could provide new options for cell-based therapeutics with curative intent. 12. Outpatient pain clinic and intranasal fentanyl to improve sickle cell disease outcomes Pediatr Blood Cancer. 2020 Aug 15;e28648. doi: 10.1002/pbc.28648. Online ahead of print. Authors Raven Myrick 1 , Shaundra Blakemore 2 , Emily Waite 1 , Brandi Pernell 3 , Avi Madan-Swain 3 , Lee Hilliard 3 , Jeffrey Lebensburger Abstract Background: Acute pain events are a leading complication for sickle cell patients. In an attempt to improve pain outcomes, we developed an outpatient pain clinic, and included intranasal fentanyl in the opioid emergency department (ED) pain order set. We evaluated admission rates and opioid administration for patients that attended both the outpatient pain clinic and ED within a 3-month period. Methods: We recorded the admission rate, IV morphine equivalents, and time from triage for each opioid order and administration from both an outpatient pain clinic and ED visit within a 3-month period for an individual pediatric patient with sickle cell disease. Results: Thirty patients received acute pain management in both settings. We identified a significant reduction in hospital admission when patients received care in the pain clinic as compared to the ED (17% vs 43%, P = .02). Additionally, outpatient pain clinic patients received significantly less IV morphine equivalents than patients received in the ED (5.6 vs 10.6 IV morphine equivalents, P < .0001). In the ED, intranasal fentanyl was administered in a significantly shorter time than patients ordered intravenous opioid (43 vs 75 min, P = .02). The mean time to receiving an opioid in the outpatient pain clinic was 57 min. Conclusion: The use of an outpatient pain clinic can reduce admission rates as compared to the ED. The use of intranasal fentanyl reduced the time to first opioid administration in the ED. Patient-centered research or quality improvement projects should continue to focus on novel approaches to acute pain event management. Keywords: fentanyl; outcomes; pain; sickle cell disease. © 2020 Wiley Periodicals LLC. 20 references 13. Medical marijuana certification for patients with sickle cell disease: a report of a single center experience Blood Adv. 2020 Aug 25;4(16):3814-3821. doi: 10.1182/bloodadvances.2020002325. Authors Susanna A Curtis 1 , Dana Lew 2 , Jonathan Spodick 3 , Jeanne E Hendrickson 4 , Caterina P Minniti 5 , John D Roberts 6 Abstract More than one-third of adults with sickle cell disease (SCD) report using cannabis-based products. Many states list SCD or pain as qualifying conditions for medical marijuana, but there are few data to guide practitioners whether or whom should be certified. We postulated that certifying SCD patients may lead to a reduction in opioid use and/or health care utilization. Furthermore, we sought to identify clinical characteristics of patients who would request this intervention. Retrospective data obtained over the study period included rates of health care and opioid utilization for 6 months before certification and after certification. Patients who were certified but failed to obtain medical marijuana were compared with those who obtained it. Patients who were certified were invited to participate in a survey regarding their reasons for and thoughts on certification. Patients who were certified for medical marijuana were compared with 25 random patients who did not request certification. Fifty adults with SCD were certified for medical marijuana and 29 obtained it. Patients who obtained medical marijuana experienced a decrease in admission rates compared with those who did not and increased use of edible cannabis products. Neither group had changes in opioid use. Patients who were certified for medical marijuana had higher rates of baseline opioid use and illicit cannabis use compared with those who did not request certification. Most patients with SCD who requested medical marijuana were already using cannabis illicitly. Obtaining medical marijuana decreased inpatient hospitalizations. 14. Building access to care in adult sickle cell disease: defining models of care, essential components, and economic aspects Blood Adv. 2020 Aug 25;4(16):3804-3813. doi: 10.1182/bloodadvances.2020001743. Authors Julie Kanter 1 , Wally R Smith 2 , Payal C Desai 3 , Marsha Treadwell 4 , Biree Andemariam 5 , Jane Little 6 , Diane Nugent 7 8 , Susan Claster 7 9 , Deepa G Manwani 10 , Judith Baker 7 , John J Strouse 11 12 , Ifeyinwa Osunkwo 13 , Rosalyn W Stewart 14 , Allison King 15 , Lisa M Shook 16 17 , John D Roberts 18 , Sophie Lanzkron 19 Abstract Sickle cell disease (SCD) is the most common inherited blood disorder in the United States. It is a medically and socially complex, multisystem illness that affects individuals throughout the lifespan. Given improvements in care, most children with SCD survive into adulthood. However, access to adult sickle cell care is poor in many parts of the United States, resulting in increased acute care utilization, disjointed care delivery, and early mortality for patients. A dearth of nonmalignant hematology providers, the lack of a national SCD registry, and the absence of a centralized infrastructure to facilitate comparative quality assessment compounds these issues. As part of a workshop designed to train health care professionals in the skills necessary to establish clinical centers focused on the management of adults living with SCD, we defined an SCD center, elucidated required elements of a comprehensive adult SCD center, and discussed different models of care. There are also important economic impacts of these centers at an institutional and health system level. As more clinicians are trained in providing adult-focused SCD care, center designation will enhance the ability to undertake quality improvement and compare outcomes between SCD centers. Activities will include an assessment of the clinical effectiveness of expanded access to care, the implementation of SCD guidelines, and the efficacy of newly approved targeted medications. Details of this effort are provided. © 2020 by The American Society of Hematology. 15. Sickle Cell Trait and Risk of Ischemic Stroke in Young Adults Stroke. 2020 Aug 12;STROKEAHA119028404. doi: 10.1161/STROKEAHA.119.028404. Online ahead of print. Authors Rebecca V Zhang 1 , Kathleen A Ryan 2 3 , Haley Lopez 1 3 , Marcella A Wozniak 1 3 , Michael S Phipps 1 3 , Carolyn A Cronin 1 3 , John W Cole 1 3 , Tara M Dutta 1 , Prachi Mehndiratta 1 , Melissa Motta 1 , José G Merino 1 , Steven J Kittner 1 3 Abstract Background and purpose: Approximately 8% of Blacks have sickle cell trait (SCT), and there are conflicting reports from recent cohort studies on the association of SCT with ischemic stroke (IS). Most prior studies focused on older populations, with few data available in young adults. Methods: A population-based case-control study of early-onset IS was conducted in the Baltimore-Washington region between 1992 and 2007. From this study, 342 Black IS cases, ages 15 to 49, and 333 controls without IS were used to examine the association between SCT and IS. Each participant’s SCT status was established by genotyping and imputation. For analysis, χ2 tests and logistic regression models were performed with adjustment for potential confounding variables. Results: Participants with SCT (n=55) did not differ from those without SCT (n=620) in prevalence of hypertension, previous myocardial infarction, diabetes mellitus, and current smoking status. Stroke cases had increased prevalence in these risk factors compared with controls. We did not find an association between SCT and early-onset IS in our overall population (odds ratio=0.9 [95% CI, 0.5-1.7]) or stratified by sex in males (odds ratio=1.26 [95% CI, 0.56-2.80]) and females (odds ratio=0.67 [95% CI, 0.28-1.69]). Conclusions: Our data did not find evidence of increased risk of early-onset stroke with SCT. Keywords: odds ratio; prevalence; risk factors; sickle cell trait; stroke; young adult. 16. Serum albumin is independently associated with higher mortality in adult sickle cell patients: Results of three independent cohorts PLoS One. 2020 Aug 10;15(8):e0237543. doi: 10.1371/journal.pone.0237543. eCollection 2020. Authors Mehdi Nouraie 1 , Allison E Ashley-Koch 2 , Melanie E Garrett 2 , Nithya Sritharan 3 , Yingze Zhang 1 , Jane Little 4 , Victor R Gordeuk 5 , Mark T Gladwin 1 3 , Marilyn J Telen 2 , Gregory J Kato 1 Abstract Sickle cell disease (SCD) impacts liver and kidney function as well as skin integrity. These complications, as well as the hyperinflammatory state of SCD, could affect serum albumin. Serum albumin has key roles in antioxidant, anti-inflammatory and antithrombotic pathways and maintains vascular integrity. In SCD, these pathways modulate disease severity and clinical outcomes. We used three independent SCD adult cohorts to assess clinical predictors of serum albumin as well its association with mortality. In 2553 SCD adult participants, the frequency of low (<35 g/L) serum albumin was 5%. Older age and lower hemoglobin (P <0.001) were associated with lower serum albumin in all three cohorts. In age and hemoglobin adjusted analysis, higher liver enzymes (P <0.05) were associated with lower serum albumin. In two of the three cohorts, lower kidney function as measured by Glomerular Filtration Rate (P<0.001) was associated with lower serum albumin. Lower serum albumin predicted higher risk of tricuspid regurgitation velocity ≥ 2.5 m/s (OR = 1.1 per g/L, P ≤0.01). In all three cohorts, patients with low serum albumin had higher mortality (adjusted HR ≥2.9, P ≤0.003). This study confirms the role of serum albumin as a biomarker of disease severity and prognosis in patients with SCD. Albumin as a biomarker and possible mediator of SCD severity should be studied further. 38 references 1 figure Full-text links |
Meetings for the Sickle Cell Community
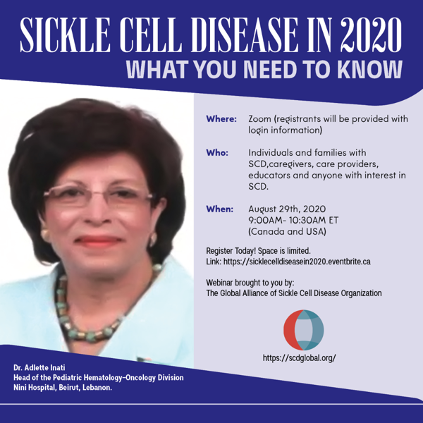
Space is limited, to attend register online: https://sicklecelldiseasein2020.eventbrite.ca
2020 Indiana Sickle Cell Conference “Sickle Cell Trait: Taking a Closer Look” The new date September 25th. This one-day Sickle Cell Disease conference will feature educational sessions for healthcare providers, patients/families, and social services providers. The morning sessions will be devoted to healthcare providers and the afternoon sessions will be tailored for patients, family members and social workers. Medically oriented topics will include improving awareness about Sickle Cell Trait and some of the health complications that research indicates can be associated with it. Health care providers and others will be presented with information that will broaden current thinking about the prevalence of trait and its impacts on the human body. Patient oriented topics will include sessions on trait education, including the variant Sickle Cell genotypes and inheritance patterns. Both sessions are open to the public. All attendees will be provided with information about available resources and current trends in the field.
registration link… https://www.eventbrite.com/e/2020-indiana-sickle-cell-conference-tickets-95286583737
First IASCNAPA Conference
The International Association of Sickle Cell Nurses and Professional Associates (IASCNAPA) Sickle Cell Conference: Treating the Whole Person scheduled for 4/17/2020 in Memphis is cancelled due to COVID-19 concerns. The decision to cancel the conference took into account many important factors, including the risk of unnecessary exposure to our patient population.
The event is rescheduled for April 9, 2021 at the Memphis Hilton.
Your understanding and support are greatly appreciated! For information go to www.iascnapa.org
Foundation for Sickle Cell Disease Research Symposium
Due to the unprecedented Novel Coronavirus COVID-19, our annual in-person Symposium is rescheduled to September 23 – 25, 2020.
The Foundation for Sickle Cell Disease Research (FSCDR) is committed to supporting innovative research in sickle cell disease (SCD) to help maximize quality of life and improve survival for the generations of people affected by SCD. The Symposium focuses on interactive education, sharing of best practices, and exploring novel Learn more and register today. https://fscdr.org/the-symposium/
NHLBI Annual Sickle Cell Disease Meeting
The National Heart, Lung, and Blood Institute’s (NHLBI) Division of Blood Diseases & Resources’ Annual Sickle Cell Disease (SCD) Meeting will be held virtually beginning on August 10, 2020 and ending on August 12, 2020. The three-day meeting provides a yearly forum for investigators, practitioners, and interested health care providers to discuss the progress of ongoing clinical trials, hear presentations about new developments in scientific and clinical aspects of SCD, and interact with other investigators and NHLBI Program Staff in an informal setting. To learn more about the meeting and register, please click here.
Virtual Sickle Cell Disease Therapeutics Conference on September 15, 2020
Global Blood Therapeutics (GBT) and the Sickle Cell Disease Association of America (SCDAA) are excited to announce that the 9th Annual Sickle Cell Disease (SCD) Therapeutics Conference (SCDTC) has been scheduled for Tuesday, September 15 starting at 9:00 AM ET. SCDAA’s President and CEO Beverley Francis-Gibson will host this event virtually. This annual event convenes key SCD stakeholders focused on discussing issues impacting the community, including the latest advancements and trends in treating sickle cell. Conference attendees will hear from innovative industry leaders, patients, physicians, community-based organizations and biotech companies. This year’s moderators include: Dr. Biree Andemariam and Mary Bentley LaMar to name a few.
This event is open to anyone with an interest in sickle cell and there will be multiple ways to attend! Sickle Cell Warriors has again exclusively partnered with GBT to livestream the conference via Facebook Live, YouTube, and Sickle Cell Warrior’s website. To learn more about the SCDTC or to register (U.S. only) visit scdconference.com. #SCDTC.

Save the Date – SCDAA’s 48th Annual National Convention 2020 Is Going Virtual
Given the current uncertainty regarding COVID-19 and its implications for attendee safety and travel, as well as for public health concerns, the Sickle Cell Disease Association of America’s (SCDAA) 48th Annual National Convention is moving to a virtual gathering on October 14-17, 2020. Clear here for more information.


